A toothache feels small compared to heart disease or cancer. Many people ignore it, delay treatment, or rely on just painkillers and feel safe. That decision can be dangerous.
Yes, a tooth infection can kill you rarely, but realistically. Modern medicine prevents most deaths, yet untreated dental infections still turn fatal every year. Understanding how this happens can save lives.
This article explains the science, risks, symptoms, and facts behind tooth infections in a clear, honest way without fearmongering or myths.
What Is a Tooth Infection?
A tooth infection, also called a dental abscess or inflammation, occurs when bacteria enter the inner pulp of a tooth. This pulp contains nerves and blood vessels. Once infected, pus forms and pressure builds.
Common causes include:
- Untreated cavities
- Cracked or broken teeth
- Gum disease
- Failed dental work
According to the Centers for Disease Control and Prevention (CDC), a dental abscess is a bacterial infection that can spread beyond the mouth if left untreated.
A tooth infection does not heal on its own. Pain may fade, but the infection often worsens silently.
Can a Tooth Infection Really Kill You?
Answering the question is simple, and yes. A tooth infection can become fatal when bacteria spread beyond the tooth into critical areas of the body.
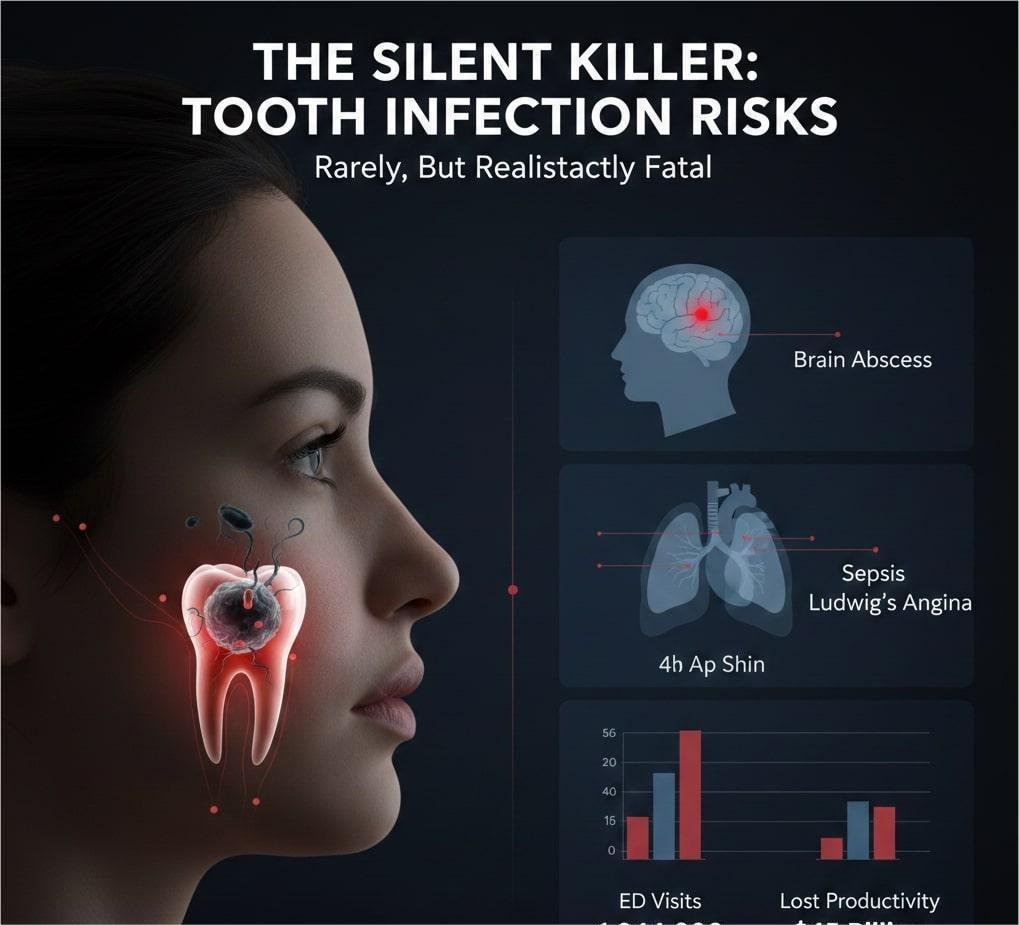
The CDC and Cleveland Clinic confirm that untreated dental infections may spread to:
- The bloodstream (sepsis)
- The brain (meningitis or brain abscess)
- The neck and airway (Ludwig’s angina)
Although death remains rare, documented cases exist even among young, healthy adults.
Tooth disorders accounted for an annual average of 1,944,000 ED visits during 2020-2022. On average, more than $45 billion in U.S. productivity is lost each year due to untreated dental disease. Oral disease can cause pain and infections, which lead to unplanned visits for emergency care, especially among those who do not have access to routine dental care. This report uses data from the National Hospital Ambulatory Medical Care Survey (NHAMCS) to study emergency department (ED) visits with either a reason for visit or diagnosis of a tooth disorder in 2020-2022.
A detailed report can be found here: https://www.ncbi.nlm.nih.gov/books/NBK615762/
How a Tooth Infection Becomes Life-Threatening
 A tooth sits close to vital structures. Once bacteria escape the tooth, they move fast.
A tooth sits close to vital structures. Once bacteria escape the tooth, they move fast.
- Sepsis (Blood Infection)
Bacteria enter the bloodstream, triggering an overwhelming immune response. Organs begin to fail.
Symptoms include:
- High fever
- Rapid heartbeat
- Confusion
- Low blood pressure
Sepsis is a medical emergency.
- Brain Infection
Upper tooth infections can spread to the sinuses and brain.
Brain abscesses cause:
- Severe headache
- Vomiting
- Vision problems
- Seizures
- Airway Blockage (Ludwig’s Angina)
Infections from lower teeth may spread under the tongue and neck.
Swelling can block breathing within hours.
Dentists describe Ludwig’s angina as one of the most dangerous dental complications.
How Long Does It Take for a Tooth Infection to Kill You?
There is no fixed timeline.
In minor cases, an infection may remain localised for weeks. In severe cases, people have died within 24 to 72 hours after symptoms escalated.
Factors that increase risk:
- Delayed treatment
- Diabetes
- Weakened immune system
- Smoking
- Poor oral hygiene
Even healthy individuals are not immune.
We will explore timelines in detail in the supporting article:
“How Long Until a Tooth Infection Kills You?”
Warning Signs You Should Never Ignore
Seek urgent dental or medical care if you notice:
- Severe, throbbing tooth pain
- Swelling of face, jaw, or neck
- Fever above 101°F (38.3°C)
- Difficulty swallowing or breathing
- Bad taste or pus in the mouth
- Fatigue with confusion
Pain suddenly stopping can mean the nerve has died, not that the infection resolved.
That silence can be dangerous.
Are Tooth Infections Contagious?
No, you cannot “catch” a tooth infection like a cold.
However, the bacteria that cause cavities and gum disease can spread through saliva, especially among children and partners. That increases cavity risk, not instant infection.
The infection itself remains local to the affected person.
Why Antibiotics Alone Are Not Enough
Many people assume antibiotics will cure a tooth infection.
Antibiotics reduce bacterial load but cannot remove the infected tissue inside the tooth. Without dental treatment, the infection often returns, in some cases even stronger.
Definitive treatments include:
- Root canal therapy
- Abscess drainage
- Tooth extraction
Dentists combine procedures with antibiotics when needed.
How Dentists Diagnose Tooth Infections
Dentists use:
- Dental X-rays
- Physical examination
- Pain response testing
X-rays reveal bone loss and abscess formation that patients cannot see.
Early diagnosis prevents serious complications.
How to Prevent a Dangerous Tooth Infection
Prevention works better than emergency treatment.
Key habits:
- Brush twice daily with fluoride toothpaste
- Floss once daily
- Treat cavities early
- Get dental checkups every 6–12 months
The CDC confirms routine dental care significantly reduces abscess risk.
Skipping dental visits can cost more later financially and medically.
The Bottom Line
A tooth infection can kill you, but it almost never should.
Modern dentistry treats infections effectively when patients act early. Ignoring symptoms, delaying care, or covering pain with pills increases risk.
Your mouth connects to your entire body. Treat tooth pain with the same seriousness as chest pain or high fever.
Frequently Asked Questions (FAQ)
Can a tooth infection really kill you?
Yes, a tooth infection can become fatal in rare cases if left untreated. Death usually occurs when bacteria spread beyond the tooth into the bloodstream, brain, or airway. Modern dental care prevents most deaths, but delayed treatment increases risk.
How common is death from a tooth infection?
Death from a tooth infection is uncommon, especially in countries with access to dental care. However, medical records confirm that fatal cases still occur every year, usually due to delayed treatment or underlying health conditions.
How long does it take for a tooth infection to become dangerous?
There is no fixed timeline. Some infections remain localised for weeks, while severe cases can escalate within days. In rare situations, complications have developed within 24 to 72 hours after symptoms worsened.
What are the first warning signs of a serious tooth infection?
Early warning signs include severe or throbbing tooth pain, swelling of the gums or face, fever, bad taste in the mouth, and pain when chewing. These symptoms indicate that the infection may be spreading.
Can a tooth infection go away on its own?
No. A tooth infection does not heal without treatment. Pain may temporarily decrease, but the infection usually continues to spread silently. Professional dental care is required to remove the source of infection.
Can antibiotics alone cure a tooth infection?
Antibiotics can reduce bacteria and control symptoms, but they cannot eliminate the infected tissue inside the tooth. Without procedures like a root canal, abscess drainage, or extraction, the infection often returns.
When should I go to the emergency room for a tooth infection?
Seek emergency care immediately if you experience facial or neck swelling, difficulty breathing or swallowing, high fever, confusion, or rapidly worsening pain. These signs suggest a medical emergency.
Are tooth infections contagious?
No, a tooth infection itself is not contagious. However, bacteria that cause cavities and gum disease can spread through saliva, increasing the risk of dental problems in others.
Why does tooth pain sometimes suddenly stop?
Pain may stop when the tooth nerve dies. This does not mean the infection is gone. In many cases, the infection continues to spread without pain, making the situation more dangerous.
How can tooth infections be prevented?
Regular brushing and flossing, early cavity treatment, and routine dental checkups every 6–12 months significantly reduce the risk of tooth infections. Prevention is safer and less costly than emergency treatment.
Note: “Content is written for educational purposes and reviewed against trusted medical sources.”